Social Media Posts Misinterpret Biden on mRNA Cancer Vaccines
SciCheck Digest
COVID-19 vaccines are not “being used to cure cancer,” as social media posts falsely claim, misinterpreting President Joe Biden’s reference to mRNA cancer vaccines during his State of the Union address. Biden was referring to the mRNA technology used to make the COVID-19 vaccines and being studied by researchers to treat cancer.
Full Story
The Pfizer/BioNTech and Moderna mRNA COVID-19 vaccines are the first vaccines using the messenger RNA technology to be approved for use, but they’re not the first ever developed. The history of mRNA vaccines started decades before the pandemic, and included research on mRNA cancer vaccines.

Unlike platforms used in other vaccines, the mRNA technology doesn’t directly introduce an antigen, such as a protein, into the body to trigger an immune response. Instead, mRNA encapsuled in a fatty envelope delivers instructions for cells to make proteins. The immune system responds by producing antibodies and immune cells, preparing the body to respond if it encounters these proteins again.
The research on cancer mRNA vaccines both enabled the development of mRNA COVID-19 vaccines and was accelerated by it. Now, several clinical trials are testing mRNA vaccines to fight different kinds of cancers — and some have shown promising early results.
President Joe Biden referred to this success in his State of the Union address on March 7.
“The pandemic no longer controls our lives,” he said. “The vaccine that saved us from COVID is — are now being used to beat cancer. Turning setback into comeback. That’s what America does.”
The president’s message wasn’t entirely clear. He was referring to the technology used to create the COVID-19 vaccines, not the COVID-19 vaccines themselves. Biden’s imprecise wording allowed opponents of COVID-19 mRNA vaccines to twist his message on social media, where users misinterpreted Biden’s statement to claim the president was announcing the same vaccines used for COVID-19 were now being used to fight cancer.
“BREAKING: Biden announces that the COVID vaccine is now being used to cure cancer,” an Instagram user wrote on March 8. Similarly, comedian and conservative commentator Terrence K. Williams posted a Rumble video on Facebook titled, “JESUS!! Biden said the Covid Vaccine is being used to cure CANCER!!”
Comments on the social media posts repeated the unsupported claim that mRNA COVID-19 vaccines cause cancer. As we’ve explained extensively, there’s no evidence to support that theory.
Philip Santangelo, a professor and cancer researcher at Emory University, told us he didn’t “think President Biden meant that literally” since COVID-19 vaccines “won’t help with cancer.” But Santangelo, who is leading a $24 million mRNA collaborative project funded by the federal government, said some of “the parts and pieces” of the mRNA COVID-19 vaccine — the mRNA platform — is being used in cancer vaccines to train the immune system to fight the disease.
“He wasn’t wrong,” Santangelo told us in a phone interview in reference to Biden’s words. “I mean, you are still using that technology, but you’re not using it in exactly the same way.”
In fact, in August, when announcing the funding for Santangelo’s project, called Curing the Uncurable via RNA-Encoded Immunogene Tuning, as part of the White House Cancer Moonshot initiative, Biden used similar, but more detailed, language.
“Over the past few years, COVID-19 vaccines developed using mRNA technology have saved millions of lives around the world,” Biden said at the time. “Now, a skilled team at Emory University in Atlanta will work to adapt these technologies to turn more cancers into curable diseases. This is a bold endeavor that has the potential to transform the fight against cancer and other difficult diagnoses.”
mRNA Cancer Vaccines
Although no mRNA cancer vaccine has been authorized or approved for use yet, many are being studied to treat different kinds of cancers.
“There are dozens, if not hundreds, of ideas of how the platform could be used for cancer,” Dr. James A. Hoxie, emeritus professor of medicine at the University of Pennsylvania and co-director of the Penn Institute of RNA Innovation, told us, referring to the potential of mRNA.
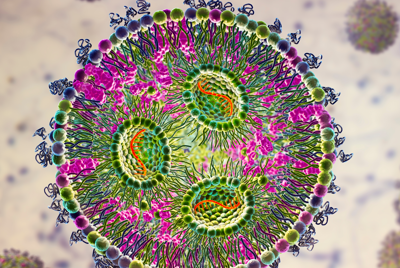 Illustration of a lipid nanoparticle containing mRNA. By Dr. Microbe / stock.adobe.com
Illustration of a lipid nanoparticle containing mRNA. By Dr. Microbe / stock.adobe.com
Therapies using mRNA rely on decades of research, in which scientists have learned how to modify RNA and package it in vesicles of fat, or lipid nanoparticles, to protect the RNA from premature degradation.
COVID-19 took the mRNA platform to “the next level,” Santangelo told us, by accelerating the manufacturing process and its scalability. The COVID-19 pandemic also created the opportunity to test the platform’s safety and efficacy in large clinical trials and evaluate the vaccines’ performance in real life.
“The production of mRNA vaccines today is easy, fast, and can be scaled up as needed,” Norbert Pardi, assistant professor of microbiology at Penn Medicine and lead of the vaccine group at the Penn Institute for RNA Innovation, told Cancer Currents, the National Cancer Institute’s blog.
Investigational cancer vaccines use the same mRNA tool as their COVID-19 predecessors — a lipid nanoparticle with RNA inside. What changes is the information the mRNA is delivering to cells. (The cancer vaccines also differ from the COVID-19 vaccines in that they’re therapeutic, meaning they’re intended to treat people who have already been diagnosed with cancer.)
Hoxie compared it to looking at two different pills that look the same, but treat different diseases. “Under a microscope, a lipid nanoparticle for COVID would look like a lipid nanoparticle to treat pancreatic cancer,” he said. “It looks the same, but they’re different.”
COVID-19 vaccines instruct cells to make spike proteins of SARS-CoV-2, the virus that causes the disease. For the cancer vaccines, scientists are using this technology to instruct cells to produce proteins that are unique to cancer cells and not present in normal cells – specifically, tumor-specific antigens and neoantigens, new proteins that occur in cancer cells when they have mutated. Both can serve as good targets for vaccines and other immunotherapy because when the immune system sees these unfamiliar antigens, the body mounts a response and produces cytotoxic T cells that destroy tumor cells.
“Essentially, you can direct your immune system — that’s why it’s called a vaccine — to kill tumor cells,” Santangelo, who is working on different vaccine models for different kinds of tumors, told us.
“mRNA is just a relatively simple way to get cells to make proteins you want them to make, that’s it,” he said. “It’s a convenient platform that can be used to either, again, introduce cancer antigen to the immune system or express things like cytokines,” which are small proteins “that can help wake the immune system and get it revved up to go kill tumor cells.”
But the development of these cancer vaccines is challenging.
The diversity of tumors and antigens is one issue. Each cancer is different, and people’s cancers have unique combinations of mutations. To address this, researchers have been trying to use mRNA that can instruct cells to produce personalized neoantigens. The mRNA is manufactured after identifying mutations in samples from a patient’s cancerous cells. The process for making a personalized mRNA vaccine usually takes between one and two months, and the vaccine can include the genetic code for up to 34 different neoantigens, according to the National Cancer Institute.
Vaccines in Clinical Trials
One of the promising vaccine candidates in the pipeline is Merck and Moderna’s personalized mRNA cancer vaccine, known as mRNA-4157 or V940, which targets melanoma, the most serious kind of skin cancer.
In a phase 2 clinical trial that involved 157 high-risk patients who had undergone surgery, 50 received the standard treatment (pembrolizumab) and 107 received standard treatment and the vaccine. Results published in January show that recurrence-free survival, which the trial was primarily intended to measure, was longer with the combination of both therapies. The rate of recurrence or death over around two years of follow-up was 22% for those who received the vaccine versus 40% for those who did not. The most common side effects from the vaccine were fatigue, chills and pain at the injection site.
In July, the companies announced a phase 3 trial, which plans to enroll “1,089 patients at more than 165 sites in over 25 countries around the world.”
“I have every confidence that this strategy will be expanded to … non-small cell lung cancer, renal cell cancer, hepatocellular cancer, gastroesophageal cancer, et cetera,” Dr. Jeffrey S. Weber, deputy director of the Perlmutter Cancer Center at NYU Langone and a trial researcher, said at a meeting of the American Association for Cancer Research, according to Medscape.
A second promising personalized mRNA vaccine, developed by BioNTech and Genentech, targets one of the most common and deadliest types of pancreatic cancer, pancreatic ductal adenocarcinoma. In a phase 1 trial, of patients who have had surgery, 15 patients were treated with a drug called atezolizumab, nine doses of a vaccine with up to 20 personalized neoantigens and standard chemotherapy drugs for pancreatic cancer.
According to the results, the vaccine activated a strong T cell response against the neoantigens in half of the patients. These patients had a longer recurrence-free survival compared with those who didn’t show a T cell expansion. A phase 2 trial of the vaccine, called autogene cevumeran, started in October 2023 and hopes to enroll 260 participants in nearly 80 sites around the world.
“The evidence from the phase 1 trial showed that we are on the right track: An mRNA vaccine can trigger T cells to recognize pancreatic cancers as foreign,” Dr. Vinod Balachandran, who led a team from the Memorial Sloan Kettering Cancer Center, said in a report from the center. “Moreover, the vaccines stimulated many such T cells, and we continued to detect T cells stimulated by such vaccines in patients up to two years later.”
Hoxie told us the results of these trials were impressive.
“In each case, it was an RNA vaccine platform that was generating an immune response that was capable of blunting, of decreasing the chance for relapse. So, what’s going to happen over time? Is that just delaying it, or is it really, totally preventing it? And, that’s what’s going to have to be seen,” he said. “But it gives you an idea why there’s excitement in the field — because you’ve done something with a vaccine that is changing the standard of care.”